In this episode, we will learn the anatomy and localisation of the brainstem lesions. The anatomy of the brainstem is often considered as difficult by medical students. In this episode, we will try to learn the brainstem anatomy from a clinical angle. We will discuss clinical cases from the midbrain, pons, and medulla and learn the anatomy of the brainstem around these cases. All students should know how to draw the midbrain, pons and medulla. We should always try to draw the lesion site on the brainstem diagram whenever we encounter a case. Please go through the images of the brainstem given on our website neurologyteachingclub.com. Students need not study all the syndromes described here. All of them are discussed to understand the anatomy of the brainstem better. At the end of this session, we will be able to
1. Draw the anatomy of the midbrain, pons and medulla.
2. Localise a lesion on the brainstem from clinical features and
3. Tell the various brainstem clinical syndromes.
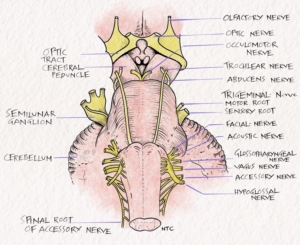
Fig-1 Base of the brain showing emergence of the cranial nerves.
While studying the anatomy of the brainstem, it is helpful to remember the ‘Rule of four’ of the brainstem. This includes
The brainstem has four midline or medial structures beginning with M, namely
1. Motor pathway or corticospinal tract
2. Medial lemniscus
3. Medial longitudinal fasciculus and
4. Motor nuclei and nerves.
The brainstem has four lateral structures beginning with S, including
1. Spinocerebellar tracts
2. Spinothalamic tract
3. Sensory nucleus of Trigeminal nerve and
4. Sympathetic tract.
There are four cranial nerves in the medulla, four in the pons, and four above the pons.
1. Four cranial nerves in the medulla- 9,10,11,12
2. Four in the pons- 5,6,7,8
3. Four above the pons- 3 and 4 in midbrain and 1 and 2 above.
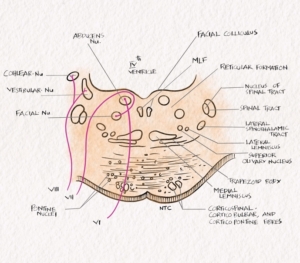
For example, let us take the case of the medulla. The medial medulla contains the four M, namely the motor pathway or pyramidal tract, the medial lemniscus, which carries fine touch, JPS from the opposite half of the body, the motor nuclei, which in the medulla is the motor nuclei of the 12th cranial nerve and the medial longitudinal fasciculus. So a medial infarct in the medulla will produce a medial medullary syndrome with weakness of opposite side due to pyramidal involvement, loss of posterior column sensations on the opposite side due to medial lemniscus involvement and ipsilateral tongue palsy due to hypoglossal involvement. Please see the image on the website the link given in the show notes. Thus, knowing the rule of four helps us understand the anatomy of the brainstem and clinical features. Similarly, a lateral medullary lesion will involve the lateral spinothalamic tract, the long tract of the trigeminal nerve, the descending sympathetic tract and cranial nerve nuclei 9,10 and 12, which we will discuss later.
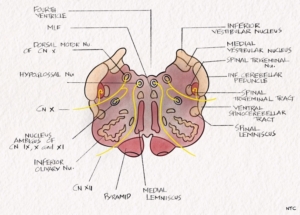
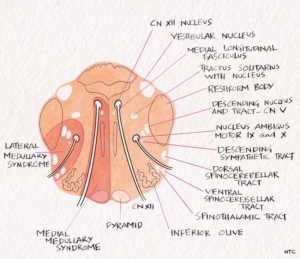
Fig- 2 Cross-section of the medulla at the mid-olivary level.
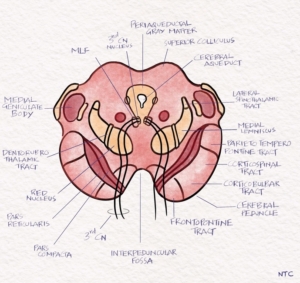
Midbrain
Let us start with the midbrain. We will have a case first. A 60-year-old male presented with acute onset weakness of the left side with right-sided ptosis on getting up in the morning. On examination, he had right 3rd CN palsy with left hemiparesis. Since the patient has a crossed hemiparesis with CN on one side and hemiparesis on the opposite side, the localisation is in the brainstem. Since the right 3rd CN is involved, the localisation is in the right midbrain. This is the classical Weber syndrome, where the third nerve fascicle and medial cerebral peduncle is affected in the anterior midbrain. The fascicle is the intra-axial part of the cranial nerve beyond the nucleus to the point it comes out of the brainstem and becomes extra-axial.
The midbrain consists of the dorsal tectum containing the colliculi, the central tegmentum containing the ascending and descending tracts, and the ventrally located cerebral peduncles containing the corticospinal and corticopontine fibres. The corticospinal tract lies in the middle 3/5 of the cerebral peduncle. Fibres in the corticospinal tract are arranged somatotopically. The fibres destined to the arm are medial, while the leg is lateral. The substantia nigra is a pigmented layer with melanin granules, dorsal to the peduncles and ventral to the red nucleus. The trochlear nerve nucleus is located in the ventral part of the central grey matter at the level of the inferior colliculus. The oculomotor nerve nucleus is located at the level of superior colliculus superior to the trochlear nucleus. The midbrain is connected to the cerebellum through the superior cerebellar peduncle. The midbrains syndromes can be divided into ventral and dorsal. The ventral syndromes include Weber, Benedikt, Claude and Nothnagel. Parinaud syndrome is the dorsal syndrome.
Fig-3 Cross-section of the midbrain at the level of the superior colliculus.
Ventral or anterior midbrain syndromes
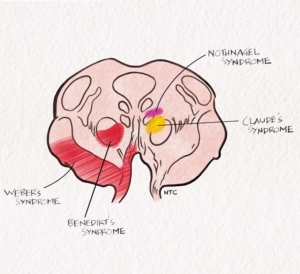
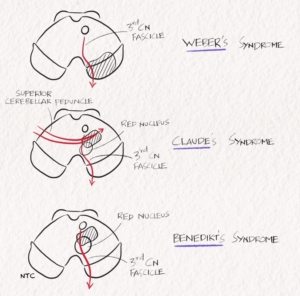
Weber syndrome
In Weber, the lesion is in the ventral midbrain involving the cerebral peduncle and third CN fascicle. The patient will have ipsilateral third CN palsy with opposite side hemiplegia.
Benedikt syndrome
The red nucleus is critical in the tremor pathway. A ventral midbrain lesion involving the red nucleus and third nerve fascicle will result in ipsilateral third nerve palsy with contralateral tremor called the Benedikt syndrome. Some patients can have hemi chorea or hemi athetosis also.
Fig -4 The ventral midbrain syndromes
Nothnagel syndrome
A lesion involving the third nerve fascicle and superior cerebellar peduncle will result in an ipsilateral third nerve with contralateral ataxia called the Nothnagel syndrome. The lesion site is more dorsal than in Benedikt syndrome.
Claude syndrome
A more extensive mesencephalic tegmental lesion involving both the red nucleus and superior cerebellar peduncle along with the third nerve fascicle will result in a combination of Benedikt and Nothnagel called the Claude syndrome. The patient will have ipsilateral third nerve palsy with contralateral tremor and ataxia. Please see the schematic diagram on the website to understand these syndromes better.
Fig-5 Schematic diagram showing the ventral midbrain syndromes
Dorsal or posterior midbrain syndrome
A 12-year-old girl presented with headache and vomiting of two weeks duration. On examination, she had vertical gaze palsy, lid retraction, convergence retraction nystagmus and light near dissociation. MRI brain showed a large pineal gland tumour compressing on the dorsal midbrain. This is the classical Parinaud’s syndrome. A dorsal rostral midbrain lesion causes it. The vertical gaze palsy is due to the involvement of riMLF and the Interstitial nucleus of Kajal in the thalamo-midbrain junction. The lid retraction and convergence retraction nystagmus are due to the loss of supranuclear inhibition to the third nerve nucleus. The light near dissociation is due to damage of the pretectal nucleus or the decussating fibres of the pretectal nucleus in the posterior commissure. The pupillary reflex will be absent, while the accommodation reflex will be present. The accommodation reflex is preserved because the accommodation pathway enters the Edinger- Westphal nucleus more ventrally. Students need to know the clinical features of dorsal midbrain lesions, which is a favourite multiple choice question for examinations. The discussion of each of these clinical features and their pathophysiology is beyond the scope of this episode. We have finished the various midbrain syndromes. Now try to draw the midbrain and mark the various midbrain syndromes, namely Weber, Benedikt, Nothnagel, Claude and Parinaud. Once you do that, you know the anatomy of the midbrain.
Pons
Once again, we will start with a case. A 70-year-old diabetic patient presented with right hemiparesis with diplopia and facial deviation to the right of one-day duration. On examination, he had right hemiparesis with Left LMN facial palsy and left lateral rectus palsy. This is the Millard Gubler syndrome characterised by ipsilateral sixth and seventh CN palsy due to fascicular lesion with contralateral hemiplegia due to lesion in the ventral caudal pons in the basis pontis.
Fig-6 The cross-section of the Pons at the level of CN 6 and 7.
The dorsal part of the pons is called the tegmentum, and the ventral portion is the basis pontis. The pontine tegmentum is mainly composed of the pontine reticular formation, a rostral continuation of the medullary reticular formation. The basis pontis contains the pontine nuclei and multidirectional nerve fibre bundles. Cranial nerve nuclei in the pons include the nucleus of the abducens nerve, located in the dorsomedial pons just beneath the floor of the fourth ventricle. Fibres from this nucleus pass ventrally between bundles of corticospinal tract fibres to exit at the pontomedullary junction. Ventromedial to the abducens nucleus is the paramedian pontine reticular formation (PPRF), which plays an important role in horizontal gaze. The motor nucleus of the facial nerve is situated ventrolaterally. The fascicle of the 7th cranial nerve winds around the 6th CN to form the facial colliculus on the floor of the fourth ventricle. The trigeminal nerve nuclei are located dorsolaterally, as are the cochlear and vestibular nuclei. The pontine lesion can be divided into ventral, dorsal and lateral pontine lesions.
Ventral or anterior pontine lesions
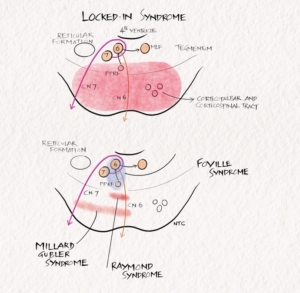
The ventral pontine lesions include Millard-Gubler, Raymond, lacunar syndromes, and Locked in state.
Millard- Gubler syndrome
A unilateral lesion in the basis pontis in the ventral-caudal pons involving the 6th CN and 7th CN fascicle and corticospinal tract results in Millard-Gubler. The patient will have ipsilateral 6th and 7th CN palsy with contralateral hemiplegia.
Raymond syndrome
A lesion in ventral medial pons involving the 6th CN fascicle and corticospinal tract. The patient will have ipsilateral lateral rectus palsy with contralateral hemiplegia.
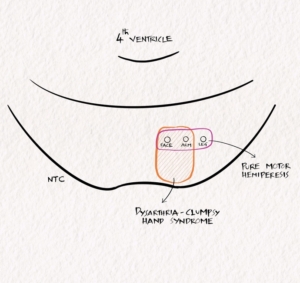
Lacunar syndromes
Small infarcts in the basis pontis can produce lacunar syndromes similar to those described in the internal capsule lesion. Basis pontis lesions can produce pure motor hemiparesis, ataxic hemiparesis and dysarthria clumsy hand syndrome.
Fig 7 Ventral pontine lacunae syndromes.
Locked-in syndrome.
Bilateral extensive ventral pontine lesion produces a locked-in state. The aetiology may be infarct, demyelination, central pontine myelinolysis etc. The patient will have quadriparesis due to the bilateral corticospinal tract involvement. The patient will have aphonia due to bilateral corticobulbar involvement. The patient will be fully conscious as the reticular activation system, located dorsally, is spared. The patient can communicate through eye blinks.
Fig 8 Schematic diagram showing the pontine syndromes.
Dorsal or posterior pontine lesions
The dorsal pontine lesion includes Foville syndrome and Raymond-Cestan syndrome.
Foville syndrome
Foville syndrome occurs with a dorsal pontine tegmentum lesion in the lower third. The 6th and 7th CN nuclei and corticospinal tract are involved. Due to corticospinal tract involvement, the patient will have contralateral hemiplegia with facial sparing. The patient will have an ipsilateral facial due to nucleus or fascicle involvement and ipsilateral gaze palsy due to PPRF or abducens nucleus involvement. The PPRF is the horizontal gaze centre which helps to look to the same side. So a patient with a Right PPRF lesion will not be able to look to the right side. When asked to look to the right, the right eye will not abduct, and the left eye will not adduct. The gaze palsy differentiates Foville syndrome from Millard Gubler, where there is only ipsilateral lateral rectus palsy due to 6th CN fascicle involvement. The supranuclear gaze palsies are a fascinating clinical discussion that requires a separate episode. I will try to make a bonus episode because it is beneficial in the clinical localisation of brain stem lesions.
Raymond-Cestan syndrome
Raymond-Cestan syndrome occurs with rostral lesions of the dorsal pons. The clinical features include ataxia with tremors due to the involvement of the cerebellum. Contralateral hypesthesia occurs due to medial lemniscal and lateral spinothalamic involvement. Contralateral hemiparesis and ipsilateral gaze palsy can occur with ventral extension.
Lateral pontine lesion.
Marie-Foix Syndrome
This syndrome is seen with lateral pontine lesions, especially those affecting the middle cerebellar peduncle. It includes ipsilateral cerebellar ataxia due to the involvement of cerebellar peduncle, contralateral hemiparesis due to involvement of the corticospinal tract and variable contralateral hemi hypesthesia for pain and temperature due to involvement of the spinothalamic tract.
Medulla
The medullary syndromes can be divided into medial and lateral. Let us discuss a case. A 55-year-old gentleman presented with sudden onset vertigo and swaying to the right of one-hour duration. He had hiccoughs, and there was nasal regurgitation when he tried to drink water. He was brought to the hospital immediately. On examination, he had right Horner’s syndrome and decreased pain on the right side of the face and the left side of the body. His gag was depressed on the right side. His power was normal, and he had right-sided cerebellar signs. The MRI brain showed a right lateral medullary infarct, and the patient improved with thrombolysis.
Fig-9 Medial and Lateral medullary syndrome
The patient has a prototype lateral medullary syndrome, otherwise called Wallenberg syndrome. Most of the major tracts and nuclei lie in the lateral medulla. It’s easier to study what is not there in the medulla. The ‘rule of four’ tells us that the 4M lies medially in the brainstem, including the motor pathway or pyramidal tract, motor nuclei of hypoglossal, medial lemniscus and medial longitudinal fasciculus. All the other long tracts and cranial nerve nuclei lie in the lateral medulla. The involvement of vestibular nuclei results in vertigo. The involvement of the inferior cerebellar peduncle results in ataxia. Swallowing difficulty and nasal regurgitation are due to the nucleus ambiguus involvement and Horner’s syndrome due to descending sympathetic tract involvement. The ipsilateral face hypoalgesia is due to the spinal tract and nucleus of the trigeminal nerve involvement. The opposite side of the body pain and temperature involvement is due to the lateral spinothalamic tract involvement. There can be an ipsilateral loss of taste due to the involvement of the nucleus of tractus solitarius. The patient can also have several eye movement abnormalities, including nystagmus, skew deviation, lateropulsion etc.
Sub medullary syndrome of Opalsky
When lateral medullary lesion extends downward into the cervical cord, ipsilateral crossed over corticospinal tract may be involved producing ipsilateral hemiplegia along with the lateral medullary syndrome. It usually occurs with vertebral artery disease.
Medial medullary syndrome of Dejerine
The ‘rule of four’ tells us that the 4M lies medially in the brainstem, including the motor pathway or pyramidal tract, motor nuclei of hypoglossal, medial lemniscus and medial longitudinal fasciculus. So a medial medullary syndrome produces opposite side weakness with loss of posterior column sensation and ipsilateral hypoglossal nerve palsy. The MLF involvement can cause upbeat nystagmus occasionally.
Hemi medullary syndrome of Babinski-Nageotte
It is a combination of the medial and lateral medullary syndrome.
That finishes this session. Try to draw the medulla and mark medial and lateral medullary syndromes. In the brainstem, one usually get excellent clinical imaging correlation, and if you have examined properly, your localisation will be correct most of the time. Next time you see a patient, try to draw the lesion before seeing the imaging. Identifying the accurate site of the lesion is more important than naming the syndrome.

Thank you so much sir