In this episode, we will discuss the clinical features of various causes of coma and the features of the different brain stem herniation syndromes. At the end of this session, we will be able to tell
1. The clinical features of metabolic encephalopathy.
2. The findings in structural causes of coma.
3. The features of various brainstem herniation syndromes
Metabolic coma
The patients with metabolic coma have clinical features depending on the particular causative illness, the depth of the coma and the comorbid illness. The developmentally newer brain structures are more susceptible to metabolic coma. So, cortical functions like cognition are lost early while brainstem reflexes like pupillary reflex remain intact until late. Similarly, complex polysynaptic pathways are affected early. Focal neurological deficits only rarely occur in a metabolic coma. Focal seizures can occur in metabolic derangement like hyperglycemia and in conditions that can break down the blood-brain barrier, like malignant hypertension and eclampsia. Toxic and metabolic encephalopathies are associated with involuntary movements like tremors, myoclonus, and asterixis.
Structural lesions above the tentorium
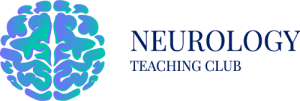
Both cerebral hemispheres must be affected to cause coma. Lesions affecting the bilateral hemisphere or bilateral thalamus can cause coma. Most of these patients will have focal neurological signs. Subarachnoid haemorrhage can present with thunderclap headache and stupor. Pituitary apoplexy can also present similarly. Unilateral supratentorial lesions like ischemia, bleeding, or tumours can cause coma due to their mass effect and secondary compression on diencephalon and upper brainstem structures. Two clinical syndromes can occur depending on the location of the intracranial lesion. A temporal or lateral extra cerebral lesion can cause an uncal herniation, while frontal, parietal and occipital lesions cause a central herniation.
Fig1- Schematic diagram showing various possible herniation syndromes due to a right sided EDH
Uncal or lateral herniation
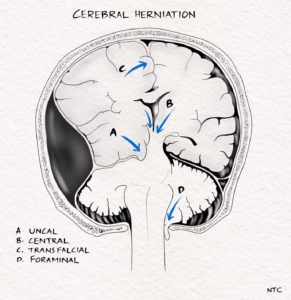
Fig-2 Early Uncal herniation due to right side EDH- Early ipsilateral third nerve compression producing anisocoria. The ipsilateral pupil is dilated and sluggishly reacting.
In patients with lateral extra-axial mass or bleeding and those with temporal lobe mass lesions and a wide tentorial opening, uncal herniation occurs. The mesial temporal lobe, the uncus anteriorly and parahippocampus posteriorly, is pushed down between the midbrain’s ipsilateral side and the tentorium’s free edge. The herniated tissue will compress the third cranial nerve and the posterior cerebral artery downward. The earliest and first symptom is usually the progressive dilatation of the ipsilateral pupil due to the third cranial nerve compression. The pupil is sluggishly reactive. This stage can last for minutes to hours, depending on the severity and acuteness of the development of the mass lesion. Prompt recognition of this state and early surgical intervention is critical in saving the patient’s life. The posterior cerebral artery compression can cause an ipsilateral occipital infarct.
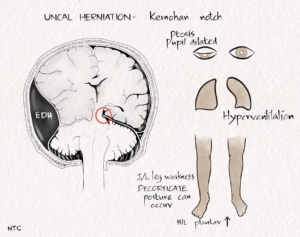
The herniated hippocampus pushes the midbrain against the thick edge of the dura on the opposite side of the tentorial opening. It produces a notch on the contralateral side of the midbrain called the Kernohan notch.
Fig-3 Uncal herniation due to right sided EDH showing Kernohan notch. The opposite side cerebral peduncle is damaged as it is pushed against the dense dura producing hemiparesis on the side of EDH
The leg fibres in the cerebral peduncle are predominantly damaged by it. As the pyramidal fibres cross over at the lower medulla, this will result in
hemiparesis in the side of the original temporal mass lesion called the Kernohan notch phenomenon. If one is not aware of this phenomenon, it can lead to a false localisation. So when a patient with hemiparesis has an ipsilateral dilated pupil, the original lesion is likely on the side of the abnormal pupil.
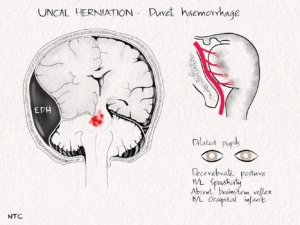
Fig-4 Late stage uncal herniation due to right sided EDH with Duret haemorrhage. There is severe damage of midbrain and pons producing decerebrate posturing and absent brainstem reflex.
In the next stage, the anteroposterior elongation and downward displacement of the midbrain cause tearing of the paramedian perforating arteries. These vessels supply the midbrain tegmentum, and the resulting infarction and haemorrhage called the Duret haemorrhage makes recovery almost impossible. The ipsilateral dilated pupil will become a little less dilated due to the damage to the sympathetic fibres. Oculomotor palsy occurs first on the ipsilateral side and later on the opposite side.
The aetiology of the uncul herniation can be surgically treated in many cases. Absent brainstem reflexes and extensor posturing before the surgery is a very poor prognostic sign. Uncul herniation survivors may be left in a locked-in or persistent vegetative state. The patient may have oculomotor dysfunction, internuclear ophthalmoplegia, vertical gaze palsy, cortical blindness and spastic limb weakness.
Central herniation
Frontal, parietal and occipital mass lesions initially compress the diencephalon and subsequently involve the midbrain, pons and medulla as the pressure increases. The clinical picture will be one of orderly rostrocaudal progression of brainstem damage termed central syndrome of rostrocaudal deterioration. The pressure effect will cause the diencephalon to shift downwards and buckle over the midbrain. It is followed by flattening of the midbrain and pons in the rostrocaudal direction resulting in elongation and rupture of the paramedian perforating arteries feeding these structures. It will result in bleeding called Durets haemorrhage and infarction in the tegmentum of the midbrain and pons.
Diencephalic stage
Impaired attention and somnolence is the earliest clinical feature. The respiratory pattern is normal, but deep sighs and yawns will occur. The pupil is small and reactive, and horizontal rowing eye movements can occur. In the late diencephalic stage, the patient cannot be aroused, and Cheyne Stokes breathing occurs. Decorticate posturing can occur. Upward gaze palsy can occur due to tectal dysfunction. Plantar is bilateral extensor. Treatment at this stage can reverse the neurological dysfunction.
Midbrain- upperpons stage
Respiration becomes quicker. Diabetes insipidus can occur due to the stretching of the median eminence of the hypothalamus. The pupil is midsized, unequal, and can be pearshaped and eccentric. The systemic release of epinephrine due to generalised anoxia can cause transient pupillary dilatation. Vertical eye movements are restricted. Decerebrate posturing can occur.
Lower pontine stage
Respiration is quick but shallow. Apneustic breathing of pontine lesion is not common in central herniation. Decerebrate rigidity decreases. Plantar bilateral extensor, with the withdrawal of legs and flexion at the knee and hip.
Medullary stage
In this late stage, ataxic breathing gives way to apnea. The pulse becomes irregular, and there will be hypotension. Large acute supraventricular lesions and Intra-ventricular bleeding can lead to sudden respiratory failure without the stepwise progression.
False localising sign
Supratentorial mass lesions in the clinically silent areas in the temporal lobe and frontal lobe and those in the midline can produce symptoms that can mislead the observer to falsely localise the lesion to the opposite hemisphere as in ipsilateral hemiplegia due to Kernohans notch. These lesions can raise the intracranial pressure and produce cranial nerve palsies that can falsely localise the lesion to the posterior fossa. Sixth cranial palsy and papilledema are the commonest false localising signs. The third, fourth, fifth, seventh and lower cranial nerve palsies can also occur.
Subtendorial structural lesions
Brainstem lesions can be easily localised clinically, as we studied in episode 9. An extensive lesion involving the brainstem, cerebellum or fourth ventricle can cause coma. Cerebellar haemorrhage is the most typical cause. Occipital headache, vomiting and ataxia are the initial symptoms. The lesion compresses the brainstem and causes other clinical signs and coma. Depending on the site of the bleed inside the cerebellum, the upper brainstem or lower brainstem can get compressed.
Lesions that compress the upper brainstem can cause upward, transtentorial herniation of the midbrain tectum and anterior cerebellar lobule. It produces coma and midbrain signs like hyperventilation, vertical gaze palsy and fixed pupil. Lower lesions compress pons and cause pinpoint pupil and lateral gaze palsy. Lower cerebellar lesions compress the medulla, producing central hypoventilation and hypotension.
Tonsillar herniation
Posterior fossa mass lesions can produce downward displacement of the cerebellar tonsil through the foramen magnum. It can cause infarction of the tonsil, medulla and upper spinal cord. The infarction is caused by anoxia and circulatory dysfunction due to medullary dysfunction.
It’s been more than ten months since we started our podcast. The podcast has been downloaded more than 15000 times from over 100 countries. It is now one of the top 10 international neurology podcasts, according to Feedspot. The link to which is given in the show notes. It brings great joy to see all the hard work paying off and see that all of you are finding it helpful. Please continue your valuable support and share it with your friends and colleagues if you find the podcast useful. Kindly write a review and provide a rating on the Apple podcast and Spotify. It will be helpful to improve the visibility of the podcast in these apps. The podcast now has value for value enabled, and you can support the show by listening on podcasting apps that support value for value, like castamatic or fountain. The images and schematic diagrams also can be directly seen in these apps.