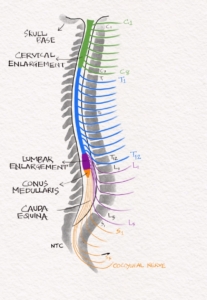
The adult spinal cord extends from the cervicomedullary junction at the upper border of the atlas vertebra to conus medullaris at the lower edge of the first lumbar vertebra. The spinal cord has a cervical, and lumbar enlargement corresponding to the upper and lower limb segmental innervation. Thirty-one pairs of spinal nerves arise from the spinal cord, including eight cervical, twelve thoracic, five lumbar, five sacral and one coccygeal. A spinal segment is a section of the spinal cord where the rootlets of a pair of spinal nerves are attached. At birth, the spinal cord lies at the L3 vertebral level. By two months, the spinal cord reaches the adult L1-L2 level.
The spinal cord length is about 45 cm in an adult male. The average length of the vertebral column is about 70cm. There is a difference between the vertebral level and spinal segmental level. The Cervical vertebrae and spinal segments are roughly corresponding. To get the segmental level in the Upper thoracic, we have to add two to the vertebral level. In the Lower thoracic, we have to add three to the vertebral level to get the corresponding segmental level. The T9-T11 vertebral level corresponds to Lumbar spinal segments L1-L5. T12-L1 vertebral level corresponds to Sacral spinal segments. The knowledge of this discrepancy between vertebral level and spinal level is essential for clinical localisation. A patient with T8 vertebral collapse compressing the spinal cord will produce sensory level at T12, the corresponding segmental level. L2 to S5 roots lie in the spinal canal below the L1 vertebra before they exit at the corresponding vertebral level. These roots form the Cauda equina. A lesion involving cauda equina will produce asymmetrical motor sensory Lower Motor Neuron syndrome. Please use the images on our website neurologyteachingclub.com or our Instagram or Facebook page of the neurology teaching club while hearing the podcast and learning the topic.
FIG 1- The vertebrae and spinal nerves
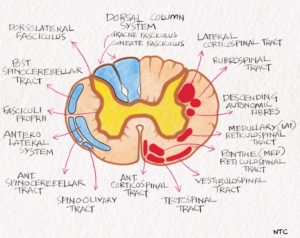
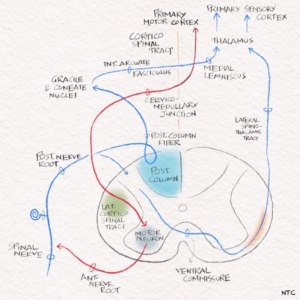
The spinal cord contains central grey, which has the cell bodies and the outer white mater, which include the long tracts. The inner grey matter is like an H or butterfly with two lateral columns joined by a transverse commissure. Each lateral column has a dorsal horn and ventral horn, which gives rise to corresponding roots. The Bell-Magendie law states that the ventral roots are motor and dorsal roots are sensory. The dorsal horn contains sensory neurons, and the ventral horn contains motor neurons. The ventral horn contains alpha motor neurons that innervate extrafusal striated skeletal muscles, the gamma motor neurons that innervate intrafusal muscle spindle fibres. There is also beta motor neurons that innervate both extrafusal and intrafusal fibres as well as the interneurons. The Central canal of the spinal cord is in the centre of the grey commissure and is lined by a single layer of endothelium.
FIG 2 – Cross-section of the spinal cord showing central grey matter and outer white matter with ascending and descending tracts
There is a small projecting lateral horn between the ventral and dorsal horn in the thoracolumbar region. It contains the intermediolateral grey column that extends from T1 to L2 gives rise to preganglionic sympathetic fibres. At S2,3,4, it contributes to the Sacral portion of parasympathetic outflow. The grey matter consists of ten Rexed laminae, the discussion of which is beyond the scope of this session.
The outer white matter has a ventral median fissure and dorsal median sulcus, dividing the cord into two halves. The exit of motor rootlets forms a pair of the ventrolateral sulcus, and the entry of sensory rootlets forms a pair of the dorsolateral sulcus. Each half of white matter is divided into three funiculi.
1. Dorsal funiculus- It is the portion of white matter between the dorsomedian and dorsolateral sulci.
2. Lateral funiculus- It is the white matter between dorsolateral and ventrolateral sulci.
3. The ventral funiculus- the white matter between ventrolateral sulcus and ventromedian fissure
They contain ascending and descending tracts. There are many ascending and descending tracts, but only three are essential from a localisation point of view. We will confine our discussion to these three tracts: lateral corticospinal, posterior column, and lateral spinothalamic tract.
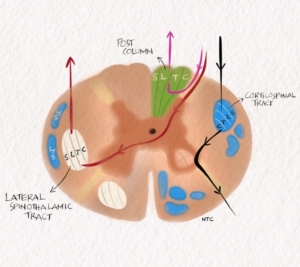
FIG 3- The three main tracts with the arrangement of fibres.
Posterior column
The posterior column carries fine touch, vibration and conscious joint position sense. Remember, the anterior spinothalamic tract carries crude touch and pressure, while the spinocerebellar tract carries unconscious proprioceptive information. The unipolar first-order neuron lies in the Dorsal root ganglia. It projects through the ipsilateral posterior column to reach the cervicomedullary junction. The fibres from the sacral area will be arranged most medially in the posterior column. The lumbar will be just lateral, followed by the thoracic. The cervical fibres are lateral most as they are the last to enter while going up. This arrangement of fibres in various tracts from medial to lateral has got clinical localisation significance. The arrangement is logically based, and there is no need to learn it by heart. The second-order neuron lies in the cuneatus and gracillis nucleus at the cervicomedullary junction and projects to the opposite thalamus. The second-order neuron immediately crosses over to the opposite side at the cervicomedullay junction as the sensory decussation. It ascends in the brainstem as the medial lemniscus to reach the thalamus. The Third-order neuron lies in the VP nucleus of the thalamus and project to the sensory cortex. Lesion of the posterior column will result in loss of vibration and JPS on the same side below the lesion. The other symptoms of posterior column involvement include
Lhermitte’s sign: It is an electric shock-like sensation down the trunk or into the arms on sudden flexion of the neck.
Paraesthesia below the level on the same side
Glove and stocking like paraesthesia
A girdle or belt-like sensation
Sensory ataxia with positive Romberg test.
Washbasin sign- increase in swaying while closing eyes as while washing face.
Lateral spinothalamic tract
The lateral spinothalamic tract carries pain and temperature sensation of the opposite side. First-order in DRG psudounipolar cells enters through dorsal horn ascends 1-2 segments and synapse with the second-order neuron in the substantia gelatinosa of Ronaldo or nucleus proprius. The second-order neuron crosses to the opposite side through the anterior commissure. It forms the lateral spinothalamic tract, which ascends through the spinal cord and brainstem to reach the opposite thalamus. The fibres from the sacral area are arranged most laterally in the lateral spinothalamic tract followed by lumbar, thoracic and cervical. The cervical fibres which are last to arrive while going up are the medial most. So an intramedullary lesion like syringomyelia will affect laterally placed sacral fibres last. The third-order neuron in the thalamus’s medial dorsal, VPL and VPM nucleus projects to the cortex. Lesion of the lateral spinothalamic tract will result in loss of pain and temperature in the opposite half of the body below the lesion level. It can also produce tract pain or funicular pain which is a deep-seated, ill localising pain. It is usually severe and difficult to characterise, distant from the affected level.
Lateral corticospinal tract
The lateral corticospinal tract carries the upper motor neuron fibres from the opposite motor cortex. It is formed by the crossed over fibres from pyramidal decussation. The first fibre to get out is the cervical. They are medial so that it is convenient for them to get out. The cervical is followed by thoracic and lumbar. Sacral fibres, which are the last to get out, is arranged most laterally in the corticospinal tract. Its again based on convenience and is easy to remember. An extramedullary compressive lesion like cervical spondylosis will affect leg fibres more than the arm, as lateral leg fibres compressed before medial arm fibres. Lesions produce UMN findings below the lesion on the same side and LMN findings at the same level. The corticospinal tract inhibits antigravity muscles and facilitates the antagonist. Lesions of the corticospinal tract produce weakness of extensors more than flexors in the upper limb and flexors more than extensors in the lower limb. Rubrospinal and lateral reticulospinal tracts inhibit antigravity muscles like the corticospinal tract. The Vestibulospinal and medial reticulospinal facilitates antigravity muscles. The corticospinal tract lesion produce a distal more than proximal weakness as well.
FIG 4- Schematic diagram of the three main tracts of the spinal cord.
Spinal cord syndromes
Now we will see the various spinal cord clinical syndromes. Knowing these is essential to localise a lesion in the spinal cord based on history and clinical findings.
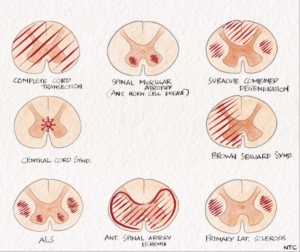
Complete transection of cord.
The spinal cord is circumferentially damaged at a level. The classic example is transverse myelitis. Both lateral spinothalamic tract and posterior column are damaged bilaterally. All sensation lost below the lesion level on both sides. The patient will have lower motor neuron findings like wasting and absent reflex at the lesion level. The patient will have upper motor neuron weakness with hypertonia, brisk reflexes and upgoing plantar below the lesion level on both sides. There may be an acute spinal shock state where lower motor neuron findings occur transiently. Polysynaptic reflexes, like bulbocavernosus first to restore after spinal shock. Bladder involved early along with constipation and erectile dysfunction.
Hemi cord transection- Brown Sequard syndrome
One half of the spinal cord is damaged, usually with an extramedullary compressive lesion. The pain and temperature will be lost below the lesion on the opposite side due to lateral spinothalamic tract involvement. The posterior column involvement results in loss of vibration and JPS on the same side below the lesion. Root pain is common. There will be LMN weakness on the same side at the level of the lesion. There will be UMN weakness below the lesion on the same side.
Central cord syndrome
The spinal cord is damaged by a lesion starting from the centre of the cord, expanding outwards. Syringomyelia and intramedullary tumours like ependymoma are typical examples. The bladder fibres are located in the centre of the cord and are involved early. The exemption to this is syringomyelia, where bladder fibres are not involved early. After the bladder, the fibres involved are crossing over pain and temperature at that level in front of the central canal. For example, if there is an intramedullary tumour arising at the C5 level, the crossing over pain and temperature fibres of both sides at that level will alone be affected. The spinothalamic tract will not be involved. This will result in loss of pain and temperature at the C5 level as the tumour is confined to C5. The crossing over pain and temperature fibres at C3 and C6 are intact. This results in suspended pain and temperature loss at the C5 level on both sides, with normal pain sensations above and below. The suspended sensory loss is a classical feature of an intramedullary lesion. The touch, vibration and JPS will be normal at C5 as the posterior column fibres do not cross over, and the central lesion has not yet involved the posterior column. There is dissociated sensory loss with pain involved but not touch and vibration. The patient can present with painless burns in the C5 dermatome or a Charcot’s joint as the patient is not aware of pain. As the tumour increase in size, the corticospinal tract will be affected. In the corticospinal tract, the cervical fibres are medial, so they are involved first. The damage to anterior horn cells in the ventral horn can present as weakness and wasting of the upper limbs. As the lesion increase in size, the dorsal column and spinothalamic tract get involved. The sacral fibres are most laterally placed in the lateral spinothalamic tract and will be the last involved. The sacral sparing is another characteristic feature of an intramedullary lesion.
Extramedullary compression
In extramedullary compressive lesions, CST, which lies in the watershed zone, is involved early. In CST, the sacral and lumbar fibres are lying outside and are involved early compared to cervical. So the patient will have increased lower-limb tone and upgoing plantar initially. The bladder fibres are involved late. Another characteristic feature of an extramedullary lesion is root pain. It is a shooting pain in the distribution of a root on coughing or straining. The extramedullary lesion can be intradural or extradural. In extradural, the lesion is outside dura, as in cervical spondylosis and vertebral metastasis. In intradural, the lesion is inside the dura as in meningioma or neurofibroma. History of neck and back pain, vertebral tenderness and vertebral deformities like gibbus or step are clinical clues to differentiate extradural from intradural lesions.
Anterior spinal artery syndrome
A single anterior spinal artery supplies the anterior two-thirds of the spinal cord, and a pair of posterior spinal arteries supply the posterior one third. The single anterior spinal artery arises from anastomosis of two branches from the vertebral artery. It runs through the entire length of the spinal cord along the anterior median fissure. The radiculomedullary arteries nourish it at a few segmental levels. The most important of which is the anterior radicular artery of Adamkiewicz that joins ASA at T9 to T12 level.
A pair of posterior spinal arteries supply the posterior 1/3 of the spinal cord. They arise from the vertebral artery or PICA. It runs through the entire length of the spinal cord. At the conus medullaris, the anterior and posterior spinal arteries are joined by anastomosing ansa of conus.
FIG 5- Blood supply of the spinal cord
ASA occlusion produces complete transection of cord but with sparing of the posterior column. The patient will have UMN findings below the lesion bilaterally. At the level of lesion, there will be LMN findings. An initial spinal shock period with LMN features below the lesion may be present. All sensations other than the posterior column are impaired below the level of the lesion. The bladder is involved early. The initial MRI spine can be normal. It is crucial to check JPS and peripheral pulses in acute paraplegia. JPS is preserved in ASA occlusion, as the posterior column is intact. The absent peripheral artery pulsation may be a clue to aortic dissection producing artery of Adamkiewicz occlusion producing ASA syndrome at the lower thoracic level. The posterior spinal artery occlusion is rare. Only the ipsilateral posterior column is affected.
Other syndromes
Posterolateral column syndrome
The posterior column and lateral corticospinal tract are involved. It is classically seen in subacute combined degeneration due to vitamin B12 deficiency. HIV myelopathy, copper deficiency and zinc toxicity are other causes for the posterolateral syndrome.
Posterior column syndrome
In posterior column syndrome, the dysfunction is limited to the posterior column. Syphilitic myelopathy is the primary cause. It can also occur as a clinically benign idiopathic condition.
Anterior horn syndrome
There is damage to anterior horn cells alone seen in conditions like SMA, poliomyelitis and Hirayama. It produces lower motor neuron findings at that level.
Anterior horn corticospinal tract syndrome
A combination of corticospinal tract damage and anterior horn cell dropout simultaneously produces upper and lower motor neuron findings. It occurs in Amyotrophic lateral sclerosis.
FIG 6- Spinal cord syndromes.
We have finished the basic anatomy of the spinal cord and the various spinal cord syndrome. In the next session, we will use this knowledge to localise the lesion in spinal cord cases. We will learn how to make a vertical and horizontal localisation in the spinal cord from the history and physical examination findings.
Excellent sessions keep going
Very useful for all clinicians to brush up and update the anatomy
Thank you
Hi, Can I just say what a relief to find someone who actually knows what theyre talking about on the internet. You definitely know how to bring an issue to light and make it important. More people need to read this and understand this side of the story. I cant believe youre not more popular because you definitely have the gift.
Thanks for your blog, nice to read. Do not stop.
very nice post, i definitely adore this website, continue it