In this session, we will learn the blood supply of the brain. We will understand the symptoms produced when a particular blood vessel is occluded. This helps to predict which artery is affected by the symptomatology of a stroke patient. Please use the images and notes of cerebral circulation on our website neurologyteachingclub.com while hearing the podcast.
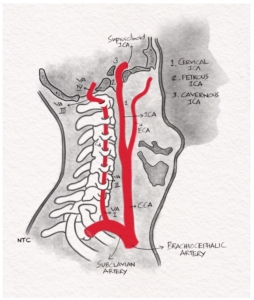
The brain’s blood supply is from two systems, the anterior and posterior circulation. The anterior circulation is formed from the right and left internal carotid artery, which arises from the corresponding common carotid artery. The right common carotid artery arises from the right brachiocephalic trunk and the left common carotid directly from the aortic arch. The posterior circulation is formed by the two vertebral arteries which arise from corresponding subclavian arteries. The two vertebral arteries join together to form the basilar artery at the pontomedullary junction. The basilar artery terminates as the two posterior cerebral arteries. The anterior and posterior circulation communicates through the posterior communicating artery, a branch of the distal internal carotid artery.
Right lateral neck view showing the ICA and the vertebral artery.
Internal carotid artery
The Common carotid artery bifurcates at the level of the C4 vertebra and the upper border of the thyroid cartilage to the External carotid artery and Internal carotid artery. The internal carotid artery lies posteriorly as a direct extension of the common carotid artery. The external carotid artery lies anteriorly and laterally. The Internal carotid artery has the following parts
1. Cervical segment
The Cervical segment ascends vertically from the bifurcation of the common carotid artery to the skull base. This segment of the internal carotid artery has no branches
2. Petrous segment
The Internal carotid artery enters the base of the skull through the carotid canal in the petrous portion of the temporal bone. The branches in this segment include the Caroticotympanic branch to the tympanic membrane and the artery of the pterygoid canal. The internal carotid artery forms an S-shaped curve called the carotid siphon. The artery crosses the foramen lacerum and enters the cavernous sinus.
3. Intracranial segment
The intracranial segment begins distal to the petrous segment and proximal to the anterior clinoid process. It has two parts.
-
- The juxta sellar or cavernous portion lies within the cavernous sinus near the Cranial nerves III, IV, VI and the ophthalmic and maxillary divisions of the CN V. The Meningohypophyseal branches arise at this level. They supply the adjacent meninges and posterior lobe of the hypophysis.
- Supraclinoid Internal carotid artery. The Internal carotid artery then pierces the dura mater medial to the anterior clinoid process, becoming the supra clinoid. The ophthalmic artery, the first major branch of the Internal carotid artery, arises at the level of the anterior clinoid process from the anterior surface. After giving off the ophthalmic branch, the Internal carotid artery gives rise to the posterior communicating artery and the anterior choroidal artery, both of which arises and course posteriorly. The posterior communicating artery joins the posterior cerebral artery to form the posterolateral portion of the circle of Willis.
After giving off the anterior choroidal artery, the Internal carotid artery terminates as the anterior cerebral and middle cerebral arteries.
Branches of the supraclinoid internal carotid artery
The ophthalmic artery
The ophthalmic artery traverses the optic canal en route to the orbit. It gives the orbital, extra orbital, and ocular branches. The most important of the ocular branches is the central retinal artery. Other ocular branches include the long and short posterior ciliary arteries and the anterior ciliary arteries. Rich anastomoses exist between the ophthalmic and the external carotid artery branches. A transient ischemic attack in the ophthalmic artery territory produces the classical clinical syndrome of Amaurosis fugax. It is a sudden onset; transient painless mono ocular visual loss described as a curtain or shade pulled down from the top or bottom of a visual field. It usually lasts for one to five minutes and rarely up to 30 minutes. The clinical significance of amaurosis fugax is that it helps differentiate between the middle cerebral artery and internal carotid artery occlusion, which produces the same symptoms of hemiplegia, hemianesthesia, hemianopia, and cortical features. Amaurosis fugax localises the disease to the internal carotid artery.
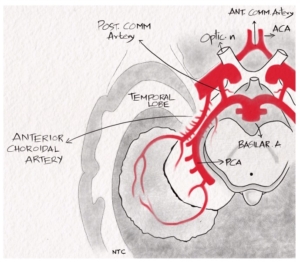
Posterior Communicating Artery
The posterior communicating artery connects the anterior with the posterior circulation and completes the circle of Willis. The posterior communicating artery supplies the anterior and posterior hypothalamus, the optic tract, posterior portion of the optic chiasm and the anterior and ventral thalamic nuclei. The clinical features of an internal carotid artery occlusion depend on the size and patency of the posterior and anterior communicating artery. For example, in a patient with a patent circle of Willis, a proximal severe right internal carotid artery stenosis can be asymptomatic. The right middle cerebral artery will get blood from posterior circulation through the patent right posterior communicating artery. The right anterior cerebral artery will get blood from the left internal carotid artery through the left anterior cerebral artery and anterior communicating artery. If it is a chronic occlusion, the internal carotid artery will also get collateral flow from the external carotid artery.
Anatomic variation of the posterior communicating artery
25% of individuals have foetal posterior communicating artery, larger than P1 and supply bulk of the blood to the posterior cerebral artery. The clinical significance of the foetal posterior communicating artery is that a middle cerebral artery occlusion can cause infarct in the posterior cerebral artery territory.
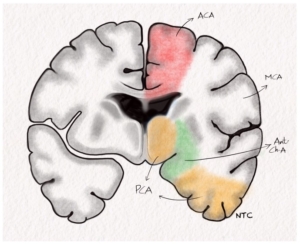
Anterior choroidal artery
The anterior choroidal artery passes posterolaterally and supplies the posterior two-thirds of the posterior limb of the internal capsule, optic tract, lateral geniculate body, optic radiation, amygdala, uncus, adjacent medial temporal lobe, posterior paraventricular corona radiata and a small supply to the thalamus. The symptoms produced by the anterior choroidal artery infarct include hemiparesis due to the posterior limb of internal capsule involvement, hemianopia due to the lateral geniculate body involvement and hemianesthesia due to thalamic supply. A middle cerebral artery infarct can cause the same triad, but the patient will be sicker and have cortical features like aphasia or neglect. There are no cortical features with an anterior choroidal artery infarct.
Basal view of the brain showing the circle of Willis and the anterior choroidal artery.
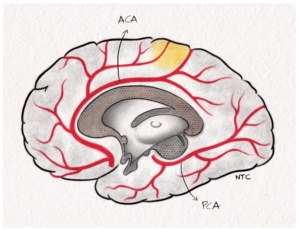
anterior cerebral artery arises below the anterior perforated substance. It runs anteromedially to the interhemispheric fissure. It joins the opposite anterior cerebral artery by way of the anterior communicating artery, closing the rostral portion of the circle of Willis. The anterior cerebral artery further follows the longitudinal cerebral fissure and courses around the genu of the corpus callosum. It continues posteriorly along the length of the body of the corpus callosum. It ends by anastomosing with callosal branches of the middle cerebral artery and the posterior cerebral artery at the splenium of the corpus callosum. Throughout its course, it gives branches that supply the medial surface of the brain.
The anterior cerebral artery can be divided into five segments
•A1 segment, which includes the proximal anterior cerebral artery up to the anterior communicating artery
•A2 or infra callosal segment, from the anterior communicating artery up to the genu of the corpus callosum.
•A3 or pre callosal segment, at the genu of the corpus callosum.
•A4 or supra callosal segment is the part above the corpus callosum.
•A5 or post callosal segment is the distal part of ACA that curves around the splenium of the corpus callosum.
Anterior cerebral artery and posterior cerebral artery in the sagittal paramedian view of the brain.
The branches of the anterior cerebral artery include
(a) the medial lenticulostriate branches,
(b) the callosal branches to the corpus callosum, and
(c) the hemispheric branches.
The medial lenticulostriate arteries
The medial lenticulostriate arteries include basal branches which supply the optic chiasm and the medial striate artery or recurrent artery of Heubner. The recurrent artery of Heubner supplies the anterior caudate nucleus and the anteroinferior part of the anterior limb of the internal capsule. It perfuses that part of the internal capsule, which supplies the face and the arm. It is prone to damage during the anterior communicating artery aneurysm clipping. Occlusion cause opposite side facio-brachial monoparesis.
The anterior cerebral artery and middle cerebral artery branches in the coronal cut of the brain.
Callosal branches
The callosal branches arise from the peri callosal artery, which is that portion of the ACA distal to the anterior communicating artery. Others reserve the term peri callosal artery for the segment beyond the origin of the calloso marginal artery.
Hemispherical branches
The hemispheric branches supply the medial surface of the hemisphere. They include the orbitofrontal, frontopolar, internal frontal Arteries, paracentral and internal parietal branches.
Areas supplied by the anterior cerebral artery.
The anterior cerebral artery supplies the anterior ¾ of the medial surface of the frontal lobe, A strip of the lateral surface of the cerebral hemisphere along the superior border and anterior 4/5 of the corpus callosum. In the motor homunculus, the leg is represented on the brain’s medial surface, which the anterior cerebral artery supplies. The paracentral lobe, essential for social continence, is also located in the anterior cerebral artery territory.
Clinical features of the anterior cerebral artery infarct
A1 occlusion
There is an occlusion of the proximal anterior cerebral artery before the anterior communicating artery. The A1 occlusion is asymptomatic as the A2 gets the blood from the opposite anterior cerebral artery through the anterior communicating artery.
Branch occlusion
Recurrent artery of Hubner
The patient will have opposite side faciobrachial monoparesis due to the internal capsule infarct.
Proximal A2 occlusion
There is an occlusion in the anterior cerebral artery just after the anterior communicating artery. The entire territory supplied by the anterior cerebral artery is infarcted. Clinical features include
-
- Opposite lower limb weakness as the leg area of the motor homunculus lies in the medial surface supplied by the anterior cerebral artery.
- Cortical sensory loss in the opposite lower limb may be present
- Incontinence due to the paracentral lobule involvement
- Grasp reflex and paratonia on the opposite side.
- Apathy, which is a lack of interest or enthusiasm.
- Transcortical motor aphasia in the left-sided lesion.
Proximal A2 with the recurrent artery of Hubner occlusion.
There is an occlusion of the anterior cerebral artery just after the anterior communicating artery and before the origin of the recurrent artery of Hubner. The clinical features include
•Opposite side hemiplegia with better recovery in the face and arm. The leg weakness due to cortical infarct has a slow recovery. The faciobrachial weakness due to internal capsule lesion has better recovery.
•Urinary incontinence and
•Apathy
Unpaired anterior cerebral artery occlusion.
In some patients, the A1 segment of one side may be absent from birth. A single A1 supplies both the anterior cerebral arteries through the anterior communicating artery. The occlusion of this only A1 produce infarct in both the anterior cerebral artery territories. The clinical features include
•Paraplegia
•Incontinence
•Abulia, which is a severe form of apathy and
•Transcortical motor aphasia
Rare syndromes with the anterior cerebral artery occlusion.
Anterior disconnection syndrome due to corpus callosal infarct.
Make the patient perform spoken commands with the right and left hands. The patient can do with the right hand but not with the left hand. This is because the left hemisphere is dominant for praxis, and the information cannot reach the right motor cortex due to the corpus callosum lesion.
An alien limb where a limb acts autonomously outside voluntary control. Apraxia and abnormal grasp play a role in this phenomenon.
Rarely choreoathetosis can occur due to caudate nucleus involvement.
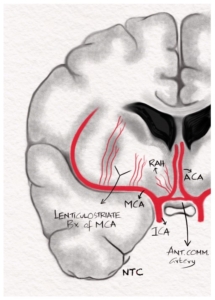
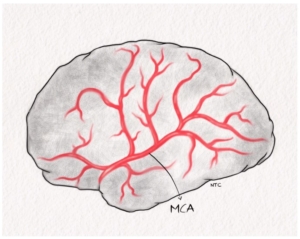
Middle cerebral artery
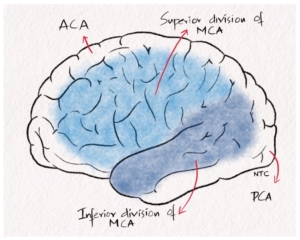
The middle cerebral artery supplies most of the lateral surface of the cerebral hemisphere and the deep structures of the frontal and parietal lobes. Three segments of the middle cerebral artery are recognised: proximal, sylvian, and distal. From the posterosuperior aspect of the proximal segment arise the penetrating lenticulostriate arteries. As the middle cerebral artery stem nears the Sylvian fissure, it gives an early anterior temporal branch and then bifurcates into a superior and inferior division. The part of the middle cerebral artery before the bifurcation is called the M1 segment. After bifurcation, M2, M3 and M4 segments represent insular, opercular and terminal cortical segments. The anterior or superior division includes the orbitofrontal, pre-central, central, and anterior parietal arteries. The posterior or inferior division comprises the posterior parietal, posterior temporal and angular arteries.
Middle cerebral artery on the lateral surface of the brain.
Clinical features of the middle cerebral artery disease
Branch occlusion
Lenticulostriate occlusion produces the classical lacunar syndromes. A lacunar stroke is a minor stroke of less than 2 cm2 in size. Depending on the location, they produce these clinical features.
Hemiplegia with infarct in the posterior limb of the internal capsule.
Hemianesthesia with the lesion in the thalamus.
Ataxic hemiparesis with the lesion in the thalamocapsular region or the posterior limb of the internal capsule
Dysarthria clumsy hand syndrome can occur with genu of the internal capsule lesion.
Superior division of the middle cerebral artery.
Superior division of the middle cerebral artery occlusion produces
Hemiparesis with the upper limb more involved
Hemisensory with sparing of the leg maybe there
Gaze deviated to the side of the lesion due to the involvement of the frontal gaze centre.
Broca’s aphasia on the left side and
Neglect or anosognosia on the right side lesion.
Inferior division of the middle cerebral artery.
Inferior division of the middle cerebral artery occlusion produces hemianopia or superior quadrantanopia of the opposite side. There will be associated Wernicke’s aphasia in the left hemisphere infarct and visuospatial difficulties and agitated delirium in the right hemisphere infarct.
Arterial supply on the lateral surface of the brain.
The middle cerebral artery stem disease
The proximal M1 occlusion is one of the most severe strokes, with around 20% mortality. The Glasgow coma scale is often poor if the entire middle cerebral artery territory is infarcted. The clinical features include
Hemiplegia
Hemianesthesia
Hemianopia
Gaze preference to the side of the lesion
Global aphasia in left hemisphere lesions
Neglect/anosognosia in right hemisphere lesions
The middle cerebral artery stem disease may lead to coma and herniation due to brain oedema.
Arterial supply of the brain in coronal cut through the thalamus.
Difference between the internal carotid artery and the middle cerebral artery occlusion.
The clinical features of the middle cerebral artery stem and terminal internal carotid artery occlusion are the same if there is poor collateral flow. The only reliable way to differentiate is if the ophthalmic artery is involved, suggesting an internal carotid artery disease.
Posterior cerebral artery.
The right and left posterior cerebral arteries are the terminal branches of the basilar artery. It supplies the occipital lobe and the infero medial temporal lobe. The proximal posterior cerebral artery up to the posterior communicating artery is called the P1 segment. The posterior cerebral artery from the posterior communicating artery to the posterior margin of the midbrain is called P2. P3 segment is from the posterior margin of the midbrain to the anterior edge of the calcarine fissure. P4 is the terminal segment where the posterior cerebral artery end as calcarine and parieto-occipital artery.
The posterior cerebral artery branches.
1. The penetrating arteries to the brainstem, thalamus, and other deep structures, including paramedian arteries, peduncular perforating arteries, thalamo perforating artery, thalamo geniculate arteries and Artery of Percheron.
2. The dorsal callosal artery supplies the splenium of the corpus callosum and anastomoses with the anterior cerebral artery.
3. The cortical branches, including the anterior temporal, posterior temporal, parieto-occipital and calcarine arteries.
4. The ventricular branches, namely medial and lateral posterior choroidal arteries.
Clinical features of the posterior cerebral artery infarct.
Branch or perforator occlusion.
The occlusion of thalamic perforators produces hemianesthesia and memory loss.
The thalamogeniculate artery supplies the thalamus and lateral geniculate body, and occlusion produces hemianesthesia with hemianopia of the opposite side.
The Artery of Percheron supplies bilateral paramedian thalamus and midbrain, occlusion of which produces memory impairment, excessive sleepiness and vertical gaze palsy due to midbrain vertical gaze centre involvement.
The disease of midbrain perforators from P1 produces the classical Weber, Claude and Benedikt syndromes which we will discuss in detail when we discuss the brainstem, which is a separate session.
The distal posterior cerebral artery occlusion
The distal posterior cerebral artery occlusion involving the calcarine artery produces opposite side macular sparing homonymous hemianopia. The macular area of the occipital cortex is supplied by a branch of the middle cerebral artery.
The posterior cerebral artery stem occlusion
The proximal P1 occlusion produces a combination of hemianesthesia with hemianopia of the opposite side with or without other perforator syndromes.
Bilateral posterior cerebral artery occlusion
Bilateral posterior cerebral artery disease usually occurs with a top of the basilar syndrome, where a thrombosis occurs at the distal basilar artery bifurcation. Bilateral posterior cerebral artery disease results in the classical Anton syndrome, where the patient has cortical blindness but won’t admit they are blind. The visual anosognosia where the patient is not aware of the visual deficit is because of the associated involvement of the visual association area in the parietal cortex. Patients often have decreased memory and agitated delirium.
Other rare posterior cerebral artery syndromes.
Left posterior cerebral artery
Alexia without agraphia, which is difficult to read without difficulty in writing, occurs with the splenium of corpus callosum lesion.
Transcortical sensory aphasia is a sensory or Wernicke’s aphasia with intact repetition.
Gerstman syndrome is due to the undercutting of the angular gyrus. The middle cerebral artery territory infarct can also produce Gerstman syndrome.
Visual agnosia
Colour anomia and transient memory impairment are the other rare clinical features of a left posterior cerebral artery infarct.
Right PCA infarct
Prosopagnosia
Disorientation
Dreams devoid of visual imagery and
Visual neglect
Rare bilateral PCA syndromes.
Balint syndrome is due to bilateral parietooccipital infarcts, which involve the dorsal or where pathways. It includes
Simultanagnosia which is an inability for a panoramic view where the patient misses the forest for the trees.
Apraxia of gaze, a difficulty in looking directly at something on instruction.
Optic ataxia, a difficulty in hand movements under the visual guide and
Decreased visual attention
The bilateral occipitotemporal pathway involving the ventral or what pathway results in prosopagnosia and defective colour vision
That finishes this session. The vertebrobasilar circulation and clinical features will be discussed, along with the discussion of the brainstem.
Excellent lecture Sir
Thank you
Very informative sir.Thanks a lot..
Thank you