Hello everyone, Welcome to the last episode of season 1 of the Clinical neurology with KD podcast. It is one year since we started our journey, and it has been nothing less than extraordinary. The podcast is now heard in over 110 countries; we had almost 18000 downloads in this period. Thank you all for this fantastic support. It means a lot. It is an amazing feeling to know that I could ignite the minds of thousands of people from different continents. At the start, I was planning 12 episodes in the first season. We ended up having fifteen. We are taking a short break before season two to come back fresher and stronger. Season 2 will be all about cranial nerves, and we will have 12 episodes again.
Meanwhile, keep sending your valuable feedback and suggestions on the NTC website, the link given in the show notes. You can also email me at neurologyteachingclub@gmail.com. I will be looking forward to hearing from you. Now let us start with the localization of bladder dysfunction.
In this session, we will learn the micturition pathways and will try to understand the clinical features of lesions involving these pathways. A localization exclusively based on urinary symptoms is often difficult, but it gives excellent corroborative evidence for neurological localization along with other symptoms, especially in spinal cord disease. At the end of this session, we will learn.
- The sympathetic, parasympathetic and somatic innervation of the bladder
- The pontine and cortical control of micturition
- The urine storage and voiding reflexes
- The signs and symptoms of lesions at various levels
The bladder has only two modes of activity, storage and voiding. An average human being passes 400-600ml of urine every 3-4 hours, and the duration of micturition is about 2-3 minutes. So 98% of the time bladder is in a storage phase. While taking history, symptoms of the dysfunction of both these phases should be asked. The symptoms of storage dysfunction include urgency, frequency, nocturia, incontinence and abnormal bladder sensation. The voiding dysfunction symptoms include hesitancy, weak stream, dysuria, intermittency, terminal dribble and need for straining to void. Post-micturition symptoms like feeling of incomplete evacuation and post-micturition dribble also need to be asked. Complete patient history should be obtained, including prior genitourinary conditions/surgeries. Medication history is significant. Sedative/hypnotic, antidepressant, antipsychotic, antihistamine, anticholinergic, antispasmodic, alpha-adrenergic agonists/antagonists, and calcium channel-blocking medications may affect voiding function. A patient urinary diary with voiding patterns, fluid intake, and voiding issues can help evaluate bladder symptoms better.
Micturition is a complex process because the autonomic nervous system and striated muscle, namely the external urethral sphincter, are involved. During the storage phase, the detrusor muscle on the bladder wall has to relax, and the external urethral sphincter has to contract so there is no incontinence. During voiding, the detrusor has to contract, and the external urethral sphincter and urethra must relax so that urine flows out without obstruction. The requirement for voluntary control over the lower urinary tract necessitates complex interactions between the autonomic nervous system mediated by sympathetic and parasympathetic nerves supplying the detrusor and urethra and the somatic mediated by pudendal nerves supplying the external urethral sphincter.
This smooth transition takes place due to coordination between
- Cortical structures
- Pontine micturition centre in the brainstem
- Ascending and descending tracts in the spinal cord
- Lumbosacral centres
- Innervation of bladder
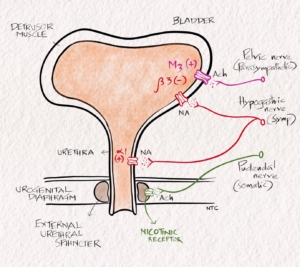
Fig 1- Innervation of bladder
The Parasympathetic innervation helps in voiding. The Parasympathetic preganglionic fibres arise from the S2–S4 spinal segments and travel in sacral roots and pelvic nerves to ganglia in the pelvic plexus and the bladder wall. Parasympathetic postganglionic axons in the pelvic nerve release acetylcholine (ACh). It produces bladder contraction by stimulating the M3 muscarinic receptors in the bladder smooth muscle.
Sympathetic innervation helps in storage. You can remember it as ‘S’ for ‘S’. Sympathetic fibres originate in the T11–L2 segments in the spinal cord and run through the Inferior mesenteric ganglia and Hypogastric nerve. Sympathetic postganglionic neurons release noradrenaline, which activates β3 adrenergic receptors to relax bladder smooth muscle. It activates α1 adrenergic receptors to contract urethral smooth muscle.
Somatic motor nerves that supply the striated muscles of the external urethral sphincter arise from the S2–S4 motor neurons called the [Onuf nucleus] and pass through the pudendal nerves. They release ACh, which produces a contraction of the external sphincter striated muscle by activating nicotinic cholinergic receptors.
Bladder sensation
Sensations of bladder fullness are conveyed to the spinal cord by the pelvic and hypogastric nerves. The pudendal and hypogastric nerves carry sensory input from the bladder neck, and urethra. They ascend in the spinal cord through the spinothalamic tract and the posterior column.
Brain areas associated with micturition include the neurons of Barrington’s nucleus (also called the pontine micturition centre (PMC), Periaqueductal grey (PAG), cell groups in the caudal and preoptic hypothalamus, the neurons of several parts of the cerebral cortex, particularly the medial frontal cortex. The pontine micturition centre is in the inhibitory control of cortical and subcortical structures, so continence is maintained during the storage phase. The cortical structures also directly control the external urethral sphincter through the corticospinal tract promoting continence.
From the micturition centre, efferents to the spinal cord descend through the reticulospinal tracts located medially and anteriorly in the anterior funiculus. They reach the detrusor motor neurons in the intermediolateral cell columns of the sacral grey matter (S2–S4). Then through the pelvic nerves, they reach the detrusor muscle.
Efferents from the cortical and subcortical centres descend through the pyramidal tracts to the pudendal nuclei (or Onuf’s nucleus) in the sacral spinal cord (S2–S4). The pudendal nerves innervate the striated muscle around the urethra.
BRADLEYS LOOPS
Bradley summarised the central sensorimotor pathways concerned with micturition and sphincter control. They are called the Bradleys loops.
- Corticospinal pathways from the motor cortex to pudendal motor neurons are concerned with the voluntary control of the sphincters and pelvic floor.
- The urethral reflex loop (from urethral afferents to pudendal motor neurons) maintains the sphincter tone when the detrusor is inactive.
- The detrusor reflex loop (from detrusor afferents to pudendal motor neurons) causes sphincter relaxation when the detrusor is active.
- The cord loop (from brainstem structures to the conus medullaris) coordinates detrusor and sphincter contraction and relaxation.
- The cerebral loop (involving the brainstem, cerebral cortex, and basal ganglia structures) initiates and inhibits switching between filling and voiding states.
- Urine storage reflex
During the storage of urine, bladder distention produces low-level afferent firing. This stimulates the sympathetic outflow in the hypogastric nerve to the bladder outlet (the bladder base and the urethra) and the pudendal discharge to the external urethral sphincter. Inhibition of the parasympathetic prevents detrusor contractions. These responses occur by spinal reflex pathways. They represent guarding reflexes, which promote continence.
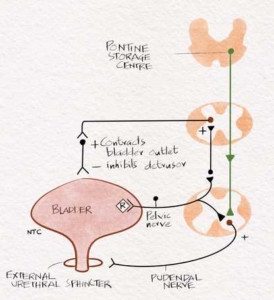
Fig -2 Storage reflex Sympathetic and somatic pudental nerve supports storage
Voiding reflex
When the bladder becomes full, intense bladder-afferent firing in the pelvic nerve activates the spinobulbospinal reflex that passes through the pontine micturition centre. This stimulates the parasympathetic discharge to the bladder and the urethral smooth muscle and inhibits the sympathetic and pudendal outflow to the urethral outlet. Relaxation of the pelvic floor and urethral sphincters occurs, accompanied by parasympathetically mediated detrusor contraction, which results in effective bladder emptying. Intact neural circuitry between the pontine micturition centre and the bladder ensures coordinated activity between the detrusor and sphincter muscles.
- Urodynamic classification
- Lapides classifies the clinical and urodynamic findings into five categories:
- Uninhibited neurogenic bladder and
- Reflex neurogenic bladder.
- Autonomous neurogenic bladder
- Motor paralytic bladder
- Sensory paralytic bladder
The naming can be a bit confusing to students. All you need to do is to know the clinical findings when there is a lesion at the various sites of the bladder pathway. The symptoms are almost predictable if you learn anatomy and physiology.
Suprapontine lesions
The disruption of the supra-pontine circuitry due to anterior cerebral lesions or the degeneration of dopaminergic neurons in Parkinson’s disease removes tonic inhibitory control over the pontine micturition centre. This will result in decreased bladder capacity and detrusor overactivity.
Hyper-reflexic or spastic neurogenic bladder
Lesion between the pontine micturition centre and sacrum causes a spastic neurogenic bladder. Loss of normal inhibition from above causes bladder contraction during filling. In most cases, the detrusor becomes overactive, so there is urinary urgency, frequency, urge incontinence and inability to initiate voluntary micturition. Small volumes of urine stimulate uninhibited detrusor contraction. The bladder capacity is reduced, but post micturition, residual urine may be increased. The bulbocavernosus and superficial anal reflexes are preserved. Simultaneous contraction of the detrusor and the sphincter during voiding, known as detrusor–sphincter dyssynergia, results in obstructed voiding, an interrupted urinary stream, incomplete emptying, and high intravesical pressures because the sphincter fails to relax correctly. Upper urinary tract dilatation and kidney damage may develop subsequently. Abnormal hyper-reflexic contractions may be poorly sustained and, in combination with dyssynergia, result in incomplete emptying.
Autonomous bladder
The autonomous bladder is seen with complete lesions below the T12 segment that involve the conus medullaris and cauda equina. It occurs with sacral myelomeningocele and tumours of the conus medullaris–cauda equina region. This is also the type of neurogenic bladder that occurs during the initial shock phase of spinal cord injury. There is detrusor areflexia. The bladder is paralyzed, and there is no awareness of the state of fullness. In most of these cases, urinary retention occurs because the tone of the detrusor muscle is abolished, and the bladder distends as urine accumulates. Inability to initiate micturition, overflow incontinence, and increased residual urine develops. There is associated saddle anaesthesia with the absence of the bulbocavernosus and superficial anal reflexes. Anal sphincter control is often similarly affected.
A motor paralytic bladder
It is seen with lesions involving the efferent motor fibres to the detrusor or the detrusor motor neurons in the sacral spinal cord. Some patients develop a motor paralytic bladder in association with lumbar spinal stenosis, lumbosacral meningomyelocele, or following radical hysterectomy or abdominoperineal resection. Patients often suffer from painful urinary retention or impaired bladder emptying. Residual urine is markedly increased. The bulbocavernosus and superficial anal reflexes are usually absent, but sacral and bladder sensations are present.
Sensory paralytic bladder
It may occur in tabes dorsalis, syringomyelia, or diabetes mellitus. It is caused by the impairment of the afferent pathways innervating the bladder or by the dysfunction of the posterior columns or lateral spinothalamic tract at the spinal cord level. Patients maintain voluntary initiation of micturition. Urinary retention, overflow incontinence, or urinary tract infection may be early symptoms. The bulbocavernosus and superficial anal reflexes may be absent, decreased, or present.
That is all in season 1. If you found the podcast helpful, write a review and give a rating on the apple podcast and Spotify. Please share the podcast with your friends and colleagues. Until we meet in season 2, it is KD signing off. Spread knowledge.